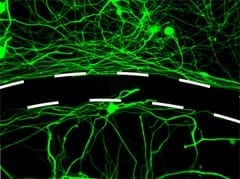
New UCLA research indicates that lost memories can be restored. The findings offer some hope for patients in the early stages of Alzheimer’s disease. For decades, most neuroscientists have b... Read more
Injections of a new drug may partially relieve paralyzing spinal cord injuries, based on indications from a study in rats, which was partly funded by the National Institutes of Health. The r... Read more