Since Prior Flu Exposure Dictates Your Future Immune Response, New Vaccine Regiments Can Be Rationally Developed, Researchers Say A team of scientists, led by researchers at The Wistar Insti... Read more
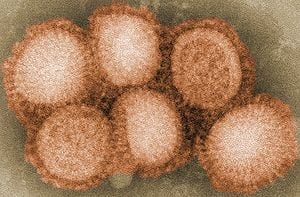
Simon Fraser University virologist Masahiro Niikura and his doctoral student Nicole Bance are among an international group of scientists that has discovered a new class of molecular compound... Read more
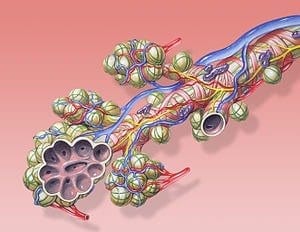
The ECLS systems are essentially artificial lungs that oxygenate the patient’s blood outside the body In recent weeks the intensive critical care units at University Health Network’s Toronto... Read more
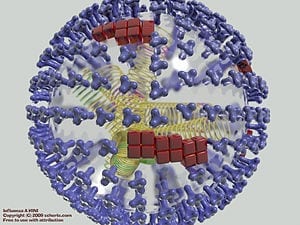
With this breakthrough the immune system can learn to recognize any type of flu virus and attack the pathogen, preventing illness. A new process to make a one-time, universal influenza vacci... Read more
It may be a particularly useful agent against pandemics and emerging viral strains In an advance toward development of a nasal spray that protects against infection with influenza and spread... Read more
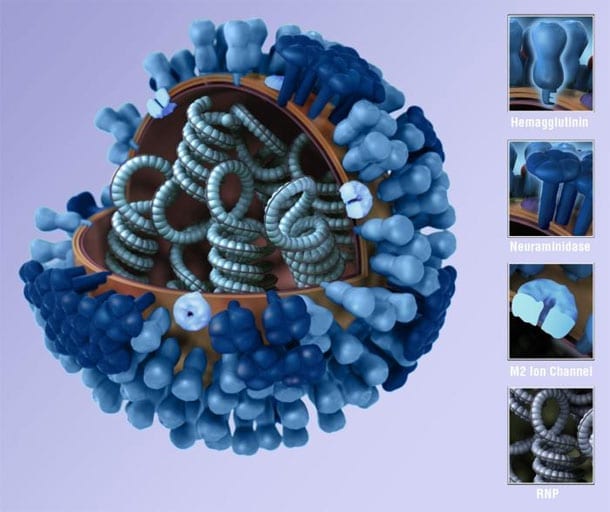
“This is indeed an exciting finding in the flu field,” I could write the entire genome of a flu virus in around 100 tweets. It is just 14,000 letters long; for comparison, our genome has ove... Read more