THOUSANDS of diabetics could be effectively “cured” thanks to a major breakthrough by Scottish scientists. Patients could now have an islet cell transplant to prevent life-threatening compli... Read more
HSCI researchers discover hormone that spurs beta cell production Researchers at the Harvard Stem Cell Institute (HSCI) have discovered a hormone that holds promise for a dramatically more e... Read more
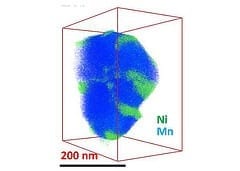
New nanotechnology can be used for Type 1 diabetes, food allergies and asthma New nanoparticle tricks and resets immune system in mice with MS First MS approach that doesn’t suppress i... Read more