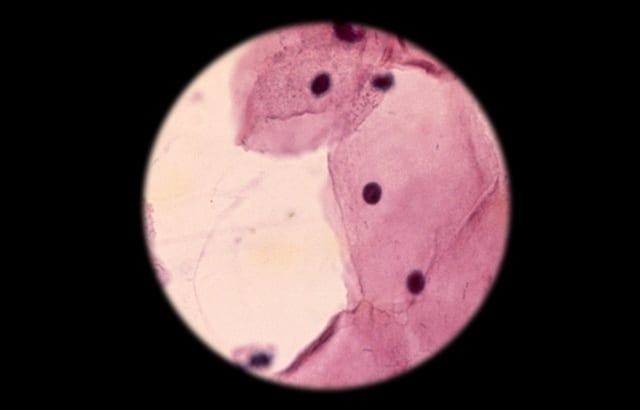
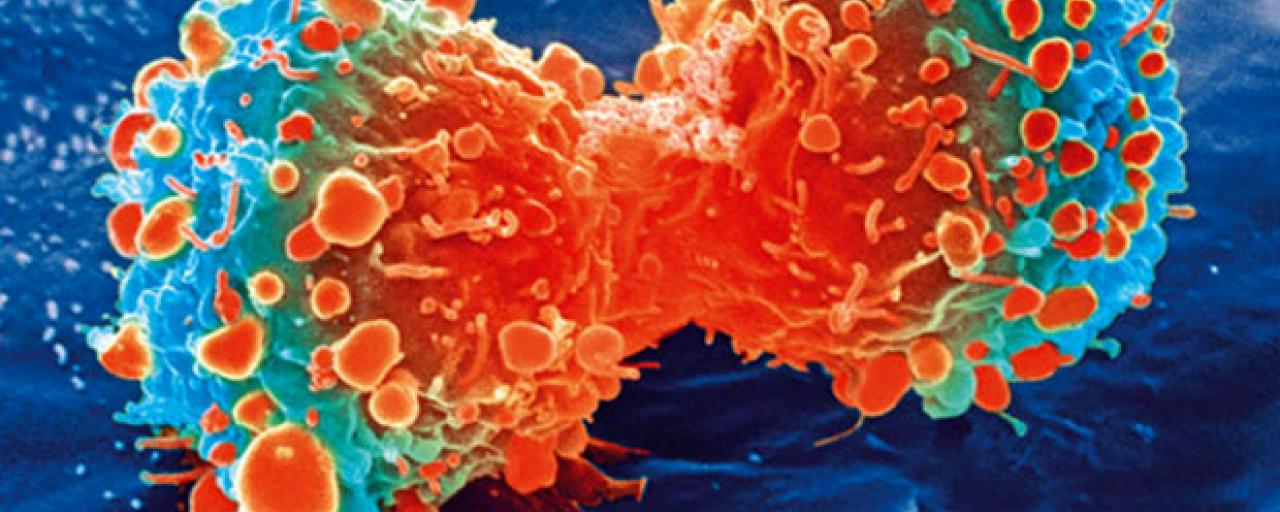
Gene-editing breakthrough in battle against cancer In what is believed to be a world first, Griffith University researchers have cured cervical cancer in mice using CRISPR gene-editing techn... Read more
A research team led by investigators from the National Institutes of Health and Global Good has developed a computer algorithm that can analyze digital images of a woman’s cervix and accurat... Read more
A new test for cervical cancer was found to detect all of the cancers in a randomised clinical screening trial of 15,744 women, outperforming both the current Pap smear and human papillomavi... Read more
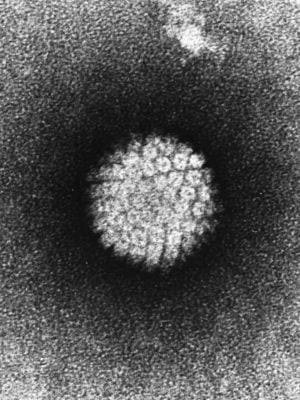
Long-term study show the nine-valent HPV vaccine greatly reduces the risk of HPV infection and HPV-associated diseases Cervical cancer is the second most common cause of cancer-related death... Read more
An artificial intelligence image detection method has the potential to outperform PAP and HPV tests in screening for cervical cancer; Low-cost technique could be used in less-developed count... Read more
There is a need to develop therapeutic vaccines for HPV-related tumors Researchers at Moffitt Cancer Center have developed and tested in mice a synthetic vaccine and found it effective in ki... Read more
Maikaew Panomyai did a little dance coming out of the examination room, switching her hips, waving her fists in the air and crowing, in her limited English: “Everything’s O.K.! Everything’s... Read more