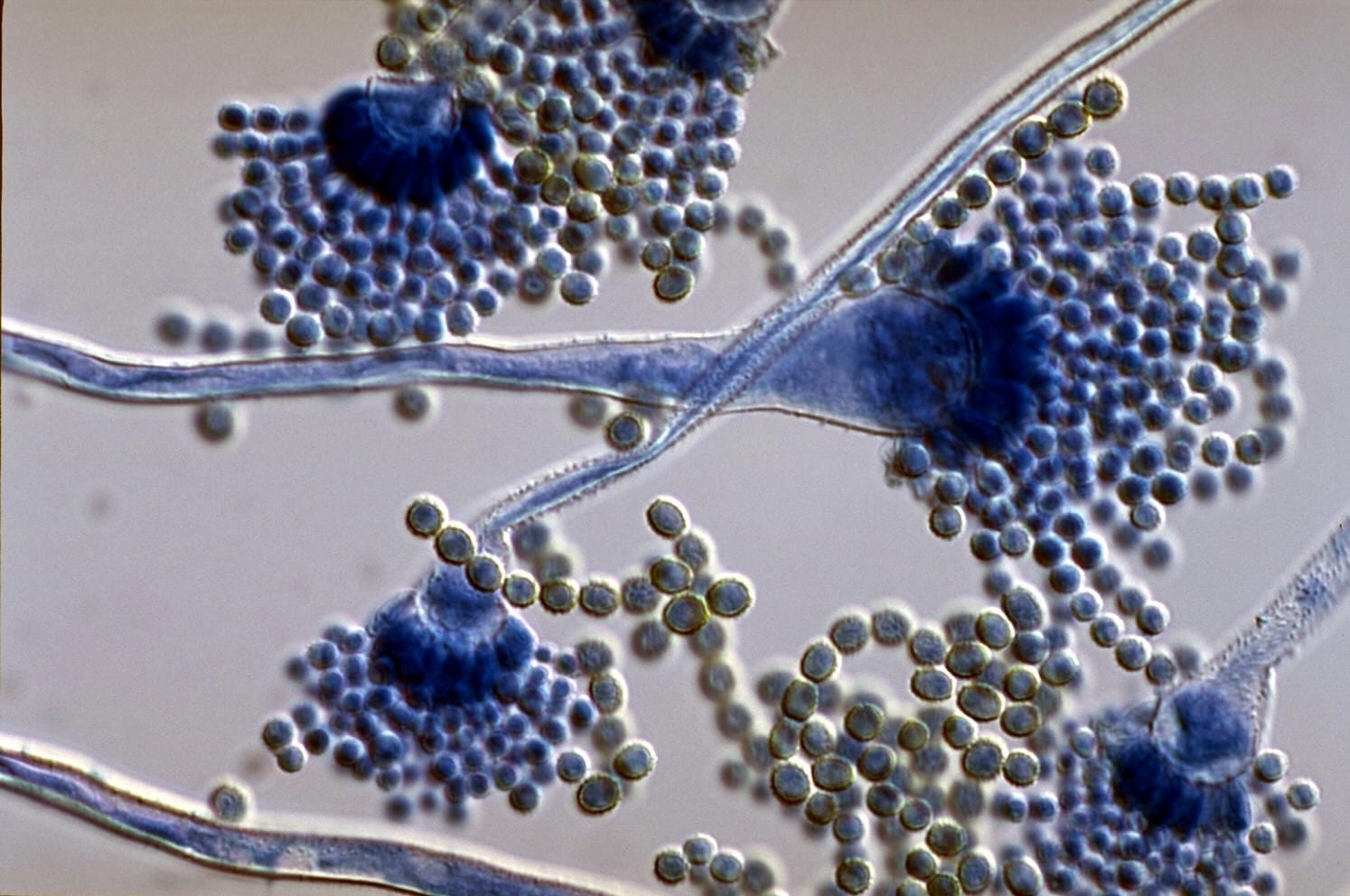
Researchers repurpose drug to deny drug-resistant fungus of iron, an element crucial to its survival How do you fight a fungal infection that is becoming increasingly resistant to medicine?... Read more
A research team at the VIB-KU Leuven Center for Microbiology has developed a novel screening method to identify antimicrobial properties of volatile substances. With this assay, they tested... Read more
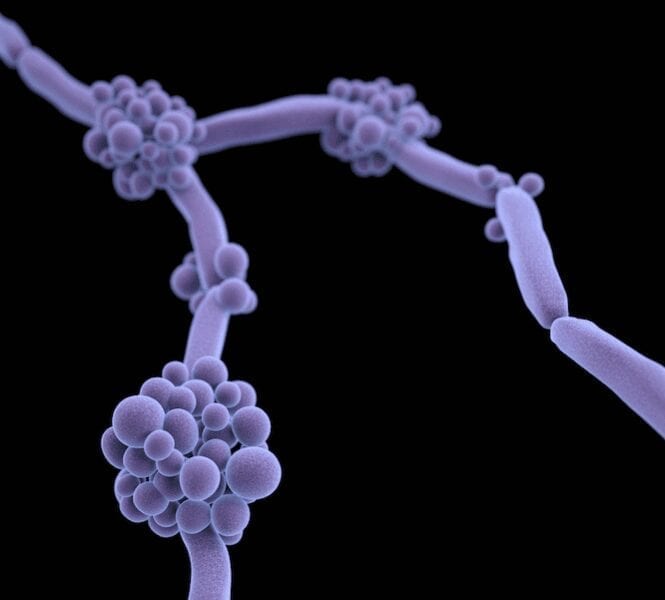
Microscopic yeast have been wreaking havoc in hospitals around the world—creeping into catheters, ventilator tubes, and IV lines—and causing deadly invasive infection. One culprit species, C... Read more
Serious fungal infections cause 1.3 million deaths annually worldwide. Researchers have identified a new class of antifungals to treat the more than 300 million people worldwide who develop... Read more